Clinical Case Summary: Sweet’s Syndrome Triggered by Inhaled Therapy
Patient Profile:
- Age/Sex: 55-year-old female
- History: Hypertension, COPD
- Lifestyle: Smoker (10 cigarettes/day), no allergies
- Medications:
- Enalapril (6 years)
- Inhaled formoterol (2 years, recently discontinued)
- New prescription: Inhaled indacaterol + glycopyrronium
Clinical Presentation:
- Timeline: Symptoms began Day 2 after starting the new inhaled therapy
- Symptoms:
- Painful, erythematous plaques on cheeks and neck
- Low-grade fever
- Notable negatives:
- No new cosmetics or foods
- No recent infections
- Recent sun exposure (with protection)
Clinical Management & Diagnosis:
- Referral: Urgent referral to Dermatology
- Investigations:
- Skin biopsy
- Blood tests: CBC, autoantibodies, lupus anticoagulant, serology
- Initial Treatment: Oral corticosteroids
Findings:
- Leukocytosis with neutrophilia
- Negative serology and autoantibodies
- Biopsy confirmed Sweet’s syndrome
Diagnosis: Sweet’s Syndrome
Also called acute febrile neutrophilic dermatosis
- Typical features:
- Sudden onset of painful, red papules or plaques (face, neck, hands, trunk)
- Systemic signs: fever, leukocytosis
- Excellent response to corticosteroids
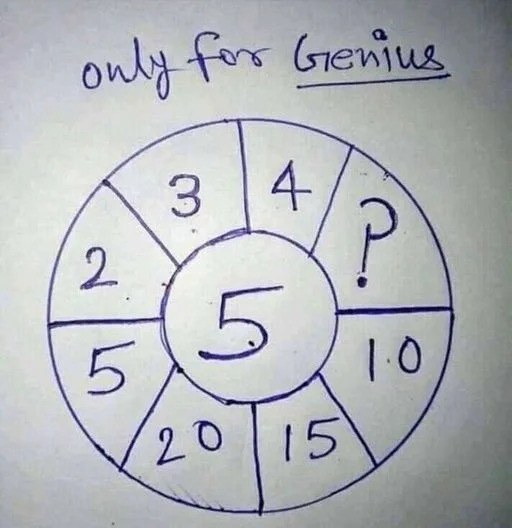
Diagnostic Criteria (Two Major + Two Minor Required):
| Major | Minor |
|---|---|
| 1. Sudden painful erythematous or violaceous plaques/nodules | 1. Fever or infection prodrome |
| 2. Neutrophilic dermal infiltrate without vasculitis | 2. Leukocytosis |
| 3. Associated arthralgia, conjunctivitis, fever, or malignancy | |
| 4. Rapid response to corticosteroids | |
| 5. Elevated ESR |
Etiology and Triggers:
- Often idiopathic or drug-induced
- Triggers include:
- Medications: contraceptives, antiepileptics, antibiotics, antihypertensives, colony-stimulating factors, vaccines
- Infections, autoimmune diseases, malignancies (especially hematologic)
- More common in women when drug-induced
✅ Novel finding: This is the first reported case of Sweet’s syndrome linked to inhaled indacaterol/glycopyrronium, highlighting the need to consider non-traditional medications as potential triggers.
Clinical Importance for Primary Care:
- Always consider Sweet’s syndrome in patients with acute onset of painful skin lesions + systemic symptoms
- Be aware of non-classic drug triggers, especially with new medications
- Initiate early referral and work-up to exclude associated malignancy, infection, or autoimmune disease
- Prompt steroid treatment leads to rapid symptom relief
Final Notes:
- Ethical guidelines followed (patient consent obtained)
- No experiments on humans or animals
- All data managed in accordance with institutional privacy policies